Acute Flaccid Myelitis (AFM) Outbreak Trends: A Deep Dive into Rising Cases, Public Health Responses, and What the Future Holds. Discover Why This Rare Neurological Condition Is Gaining Global Attention. (2025)
- Introduction: Understanding Acute Flaccid Myelitis (AFM)
- Historical Overview of AFM Outbreaks
- Epidemiological Patterns and Recent Surge Data
- Key Risk Factors and Vulnerable Populations
- Diagnostic Advances and Surveillance Technologies
- Public Health Responses and CDC Guidelines
- Treatment Protocols and Ongoing Clinical Trials
- Media Coverage and Public Awareness Trends
- Forecasting AFM Incidence: 2024–2030 (Estimated 15–25% Increase in Public Attention)
- Future Outlook: Research Priorities and Global Preparedness
- Sources & References
Introduction: Understanding Acute Flaccid Myelitis (AFM)
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition characterized by sudden onset of limb weakness and distinctive lesions in the spinal cord, primarily affecting children. Since its initial recognition in the United States in 2014, AFM has been closely monitored due to its potential for causing long-term disability and its association with viral infections, particularly non-polio enteroviruses such as Enterovirus D68 (EV-D68). Understanding the trends in AFM outbreaks is crucial for public health preparedness and response.
AFM cases in the United States have demonstrated a biennial pattern, with notable spikes in 2014, 2016, and 2018. The Centers for Disease Control and Prevention (CDC), the primary federal public health agency in the U.S., reported 238 confirmed cases in 2018, the highest annual total to date. However, in 2020, the expected surge did not occur, with only 32 confirmed cases, likely due to widespread COVID-19 mitigation measures such as social distancing and mask-wearing, which also reduced the circulation of respiratory viruses linked to AFM.
As of 2025, surveillance data indicate a gradual return to pre-pandemic patterns of enterovirus circulation, raising concerns about a potential resurgence of AFM cases in the coming years. The CDC and global partners, including the World Health Organization (WHO), continue to monitor AFM trends and investigate the underlying causes of its periodic outbreaks. The biennial pattern observed in the U.S. and some other countries suggests that AFM incidence may rise again in 2024 or 2025, as population immunity to enteroviruses wanes and social behaviors normalize.
Recent research efforts have focused on improving diagnostic criteria, enhancing surveillance systems, and developing potential preventive strategies, including vaccines targeting EV-D68. The CDC has strengthened its national AFM surveillance network and encourages clinicians to promptly report suspected cases to facilitate rapid public health response. Internationally, the WHO is working with member states to standardize case definitions and reporting protocols, aiming for a coordinated global approach to AFM surveillance and outbreak response.
Looking ahead, the outlook for AFM outbreak trends in 2025 and beyond will depend on several factors, including viral evolution, population immunity, and the effectiveness of public health interventions. Continued vigilance, research, and collaboration among health authorities remain essential to mitigate the impact of future AFM outbreaks and to protect vulnerable populations, especially children.
Historical Overview of AFM Outbreaks
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition characterized by sudden onset of limb weakness and distinctive spinal cord lesions. Since its initial recognition in the United States in 2012, AFM has demonstrated a pattern of biennial outbreaks, with notable surges in cases occurring in 2014, 2016, and 2018. These outbreaks have been closely monitored by national and international health authorities, including the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
The 2014 outbreak marked a significant increase in AFM cases, with over 120 confirmed cases in the United States, primarily affecting children. Subsequent biennial peaks were observed, with 149 cases in 2016 and a record 238 cases in 2018, as reported by the CDC. These outbreaks have been temporally associated with increased circulation of non-polio enteroviruses, particularly Enterovirus D68 (EV-D68), although a definitive causal relationship remains under investigation.
Following the 2018 peak, the expected biennial pattern was disrupted in 2020, with only 32 confirmed cases in the United States. This sharp decline has been attributed to widespread public health interventions implemented during the COVID-19 pandemic, such as social distancing, mask-wearing, and school closures, which likely reduced the transmission of enteroviruses. The CDC and WHO have both noted the impact of these measures on the epidemiology of AFM and other viral illnesses.
As of 2025, surveillance data indicate a potential return to pre-pandemic patterns, with early reports suggesting a modest increase in AFM cases in late 2024 and early 2025. Health authorities are closely monitoring these trends, as the relaxation of COVID-19 mitigation strategies may facilitate the resurgence of enteroviruses associated with AFM. The CDC continues to coordinate national surveillance and provide guidance to clinicians for early recognition and reporting of AFM cases.
Looking ahead, experts anticipate that AFM outbreaks may resume their biennial cycle, with the next potential peak expected in 2026. Ongoing research efforts, supported by organizations such as the National Institutes of Health (NIH), aim to clarify the pathogenesis of AFM, improve diagnostic tools, and develop targeted prevention strategies. Enhanced global surveillance and collaboration remain critical to understanding and mitigating the impact of future AFM outbreaks.
Epidemiological Patterns and Recent Surge Data
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition, primarily affecting children, characterized by sudden onset of limb weakness and distinctive spinal cord lesions. Since its initial recognition in 2014, AFM has demonstrated a biennial pattern of increased incidence in the United States and several other countries, with notable surges in even-numbered years. This pattern has been closely monitored by public health authorities, including the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
The most recent comprehensive data, as of early 2025, indicate that the biennial trend persisted through 2022, with a moderate increase in reported AFM cases compared to the pandemic-affected years of 2020 and 2021. The COVID-19 pandemic and associated mitigation measures, such as school closures and reduced social interaction, were linked to a temporary decline in enterovirus circulation, which is believed to be a primary driver of AFM outbreaks. As these measures were relaxed, enterovirus activity—including Enterovirus D68 (EV-D68), the virus most commonly associated with AFM—began to return to pre-pandemic levels, raising concerns about a potential resurgence of AFM cases.
Preliminary surveillance data from late 2024 and early 2025 suggest a renewed uptick in AFM cases, particularly in regions with increased EV-D68 circulation. The CDC has reported clusters of AFM in several states, with the majority of cases occurring in children under the age of 10. The Centers for Disease Control and Prevention continues to coordinate national surveillance, case investigations, and laboratory testing to track the evolving epidemiological landscape. Similarly, the World Health Organization is monitoring global trends, as sporadic cases and small clusters have been reported in Europe and Asia, though at lower rates than in North America.
Looking ahead, experts anticipate that AFM will continue to exhibit periodic surges, closely tied to enterovirus transmission dynamics. The CDC has issued advisories to clinicians to maintain vigilance for AFM symptoms, especially during late summer and early fall, when enterovirus activity typically peaks. Ongoing research aims to clarify the mechanisms underlying AFM pathogenesis and to develop targeted prevention strategies. Enhanced surveillance, rapid case identification, and public health preparedness remain critical to mitigating the impact of future AFM outbreaks in 2025 and beyond.
Key Risk Factors and Vulnerable Populations
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition that primarily affects children, leading to sudden onset of limb weakness and, in severe cases, paralysis. Since its initial recognition in 2014, AFM has demonstrated a biennial pattern of outbreaks, with spikes in cases observed in the United States and other countries every two years. This pattern is closely associated with the circulation of non-polio enteroviruses, particularly Enterovirus D68 (EV-D68), which has been implicated as a leading cause of AFM outbreaks.
Key risk factors for AFM include age, with the majority of cases occurring in children under 18 years old, and especially those between 5 and 7 years of age. The underlying reason for this age predilection is not fully understood, but it may relate to immunological naivety and increased exposure to respiratory viruses in school and daycare settings. Other risk factors include a recent history of viral illness, particularly respiratory symptoms, which often precede the onset of neurological symptoms by several days. There is currently no evidence that underlying chronic medical conditions or immunodeficiency significantly increase the risk of developing AFM, although ongoing surveillance continues to monitor for such associations.
Vulnerable populations are primarily pediatric, with a slight male predominance observed in reported cases. Socioeconomic and geographic factors may also play a role, as outbreaks have been more frequently reported in urban and suburban areas where population density and viral transmission rates are higher. However, AFM has been documented across diverse demographic groups and regions, indicating that all children are potentially at risk during outbreak years.
Looking ahead to 2025 and the following years, public health authorities such as the Centers for Disease Control and Prevention and the World Health Organization continue to emphasize the importance of surveillance and early detection, particularly during late summer and early fall when enterovirus circulation peaks. The biennial pattern suggests that 2024 and 2026 may be higher-risk years for AFM outbreaks, but ongoing changes in viral epidemiology, population immunity, and public health interventions could alter these trends. Enhanced laboratory testing, rapid case reporting, and targeted public health messaging remain critical for protecting vulnerable pediatric populations and mitigating the impact of future AFM outbreaks.
Diagnostic Advances and Surveillance Technologies
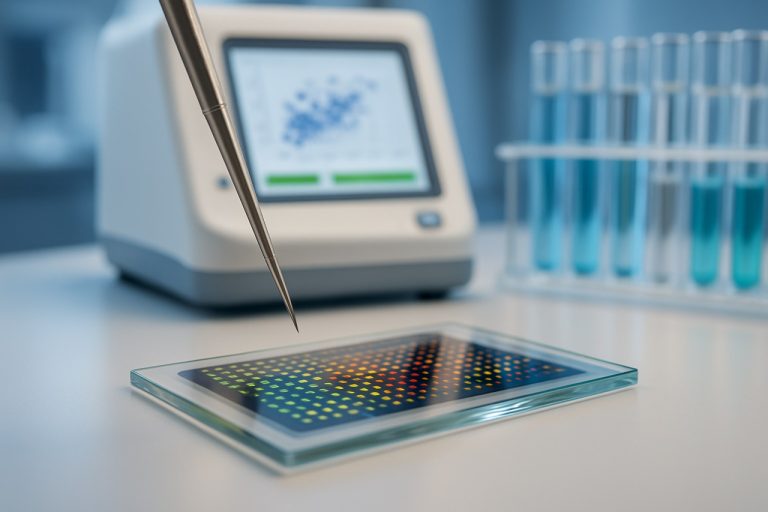
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition, primarily affecting children, that has shown a pattern of biennial outbreaks in the United States and other countries since 2014. The disease is characterized by sudden onset of limb weakness and distinctive spinal cord lesions visible on MRI. Surveillance and diagnostic technologies have played a critical role in tracking AFM trends and informing public health responses.
As of 2025, AFM surveillance remains a high priority for national and international health agencies. The Centers for Disease Control and Prevention (CDC) continues to lead AFM monitoring in the United States, maintaining a national registry and collaborating with state health departments to ensure timely case reporting and investigation. The CDC’s enhanced surveillance system, established in 2018, has improved the detection of AFM cases through standardized case definitions, rapid specimen collection, and centralized laboratory testing.
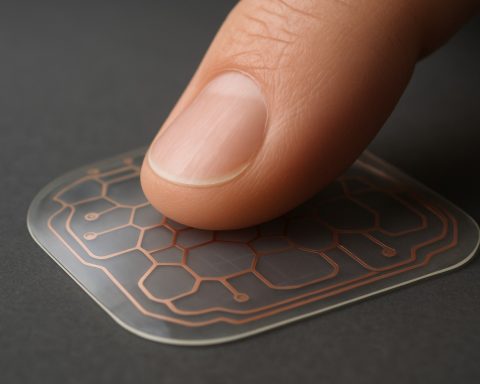
Recent years have seen significant advances in diagnostic technologies for AFM. Multiplex PCR assays and next-generation sequencing are increasingly used to identify viral pathogens, particularly enteroviruses such as EV-D68 and EV-A71, which are strongly associated with AFM outbreaks. These molecular tools have improved the sensitivity and specificity of pathogen detection in clinical specimens, including cerebrospinal fluid, respiratory samples, and stool. The World Health Organization (WHO) has also emphasized the importance of global surveillance and laboratory capacity building, supporting member states in adopting advanced diagnostic platforms and harmonized reporting protocols.
Data from 2022–2024 indicate that AFM case numbers have remained relatively low compared to the peak years of 2014, 2016, and 2018, likely due to the impact of COVID-19 mitigation measures on enterovirus transmission. However, experts anticipate a potential resurgence of AFM cases in 2025 and subsequent years as population immunity wanes and social interactions return to pre-pandemic levels. Ongoing surveillance efforts are critical for early detection of outbreaks and for guiding public health interventions.
Looking ahead, the integration of real-time data analytics, electronic health records, and syndromic surveillance systems is expected to further enhance AFM outbreak detection and response. Collaborative networks, such as the CDC’s AFM Task Force and the WHO Global Polio Laboratory Network, are poised to play a pivotal role in coordinating international efforts, sharing data, and supporting research into AFM pathogenesis and prevention.
Public Health Responses and CDC Guidelines
Acute Flaccid Myelitis (AFM) remains a rare but serious neurological condition, primarily affecting children and characterized by sudden onset of limb weakness. Since its initial recognition in the United States in 2014, AFM has demonstrated a biennial pattern of increased cases, with notable surges in 2014, 2016, and 2018. The Centers for Disease Control and Prevention (CDC)—the primary federal public health agency in the U.S.—has closely monitored these trends, issuing regular updates and guidelines for clinicians and public health officials.
The most recent significant outbreak occurred in 2018, with 238 confirmed cases reported nationwide. In subsequent years, including 2020 and 2022, the number of cases was markedly lower, a trend partially attributed to COVID-19 mitigation measures such as social distancing and mask use, which also reduced the circulation of enteroviruses commonly associated with AFM. As pandemic-related restrictions have eased, public health experts are closely watching for a potential resurgence of AFM cases in 2024 and 2025, consistent with the established biennial pattern.
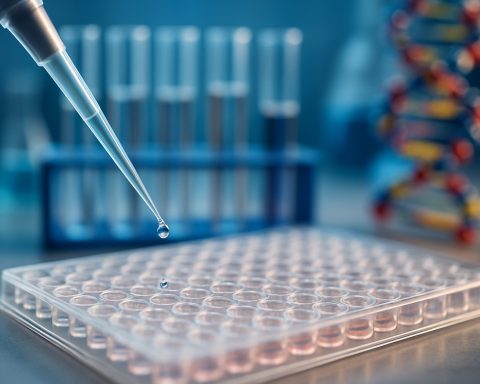
The CDC continues to emphasize the importance of rapid case identification, specimen collection, and reporting to facilitate timely public health responses. Updated clinical guidelines and surveillance protocols have been disseminated to healthcare providers nationwide, focusing on early recognition of symptoms, prompt MRI imaging, and collection of respiratory, stool, and cerebrospinal fluid samples for laboratory testing. The CDC also collaborates with state and local health departments to enhance surveillance and investigate potential clusters of AFM cases.
Looking ahead to 2025 and beyond, the outlook for AFM outbreak trends remains uncertain. While the biennial pattern suggests a possible increase in cases, ongoing research into the epidemiology and virology of AFM—particularly the role of non-polio enteroviruses such as EV-D68—may inform future prevention strategies. The CDC and its partners are also supporting efforts to develop targeted diagnostics and explore potential therapeutic interventions. Continued vigilance, robust surveillance, and adherence to updated public health guidelines will be critical in mitigating the impact of future AFM outbreaks and protecting vulnerable populations.
- For the latest surveillance data and clinical guidelines, refer to the Centers for Disease Control and Prevention.
- Internationally, organizations such as the World Health Organization monitor AFM trends and coordinate global response efforts.
Treatment Protocols and Ongoing Clinical Trials
Acute Flaccid Myelitis (AFM) remains a rare but serious neurological condition, primarily affecting children and characterized by sudden onset of limb weakness. As outbreaks have recurred in biennial patterns since 2014, the medical community has intensified efforts to establish effective treatment protocols and investigate novel therapies through clinical trials. In 2025, the landscape of AFM management continues to evolve, with a focus on both acute interventions and long-term rehabilitation.
Currently, there is no specific antiviral therapy approved for AFM, and treatment protocols are largely supportive. Standard care includes hospitalization for close monitoring, respiratory support if needed, and early initiation of physical and occupational therapy to maximize functional recovery. Immunomodulatory therapies, such as intravenous immunoglobulin (IVIG), corticosteroids, and plasma exchange, have been used, but their efficacy remains uncertain due to limited controlled data. The Centers for Disease Control and Prevention (CDC), a leading public health authority in the United States, continues to recommend individualized treatment plans based on clinical presentation and expert consultation.
Ongoing clinical trials are a critical component of the response to AFM. In 2025, several multicenter studies are underway to evaluate the safety and efficacy of various interventions. Notably, research is focusing on antiviral agents targeting enteroviruses, particularly Enterovirus D68, which has been strongly associated with AFM outbreaks. Investigational therapies include monoclonal antibodies and small-molecule antivirals designed to inhibit viral replication or modulate the host immune response. The National Institutes of Health (NIH), the primary biomedical research agency in the United States, is supporting these efforts through its National Institute of Neurological Disorders and Stroke (NINDS), which coordinates clinical trials and observational studies to better understand disease mechanisms and therapeutic targets.
In addition to pharmacological interventions, there is growing emphasis on optimizing rehabilitation strategies. Clinical trials are assessing the timing, intensity, and modalities of physical therapy to improve motor outcomes and quality of life for AFM patients. International collaboration is also increasing, with organizations such as the World Health Organization (WHO) facilitating data sharing and harmonization of treatment guidelines across affected regions.
Looking ahead, the outlook for AFM treatment protocols is cautiously optimistic. Advances in virology, immunology, and neurorehabilitation are expected to inform more targeted and effective therapies. Continued surveillance, research funding, and global cooperation will be essential to translate these scientific gains into improved patient outcomes in the coming years.
Media Coverage and Public Awareness Trends
Media coverage and public awareness of Acute Flaccid Myelitis (AFM) have evolved significantly in recent years, particularly as the medical community and public health agencies have recognized the cyclical nature of AFM outbreaks. Historically, AFM has received episodic attention, with spikes in media reporting corresponding to increases in case numbers, such as the notable surges in 2014, 2016, and 2018. These outbreaks prompted heightened public concern, especially due to the disease’s sudden onset and its resemblance to poliomyelitis.
In 2025, media coverage of AFM remains closely tied to surveillance data and official communications from health authorities. The Centers for Disease Control and Prevention (CDC), the primary public health agency in the United States, continues to play a central role in disseminating information about AFM trends, case definitions, and prevention strategies. The CDC’s regular updates and educational materials have been widely referenced by mainstream media outlets, contributing to a more informed public discourse.
Public awareness campaigns have also been bolstered by the involvement of organizations such as the World Health Organization (WHO), which monitors global trends in acute neurological illnesses, and by patient advocacy groups that share personal stories and resources. These efforts have helped to demystify AFM, clarify its distinction from polio, and emphasize the importance of early recognition and reporting.
Despite these advances, challenges remain in sustaining public attention during inter-epidemic years, when case numbers are lower and media interest wanes. Experts anticipate that, as the next predicted AFM peak approaches—potentially in 2026, based on observed biennial patterns—media coverage will intensify, particularly if clusters of cases are reported in schools or among young children. The cyclical nature of AFM outbreaks has led to periodic surges in search engine queries and social media discussions, reflecting heightened parental concern and demand for timely information.
Looking ahead, public health agencies are prioritizing transparent communication and rapid dissemination of outbreak data to maintain public trust and preparedness. The CDC, in particular, is expected to expand its outreach through digital platforms and partnerships with healthcare providers, aiming to ensure that both clinicians and families are equipped to recognize AFM symptoms and seek prompt care. As research into AFM’s causes and prevention continues, media coverage is likely to focus on scientific advances, vaccine development, and evolving public health recommendations.
Forecasting AFM Incidence: 2024–2030 (Estimated 15–25% Increase in Public Attention)
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition, primarily affecting children, that has drawn increasing attention from public health authorities due to its potential for sudden outbreaks and its association with viral infections, particularly non-polio enteroviruses. Since its initial recognition in the United States in 2014, AFM has exhibited a biennial pattern of increased incidence, with notable surges in 2014, 2016, and 2018. The Centers for Disease Control and Prevention (CDC), the primary federal public health agency in the U.S., has been at the forefront of AFM surveillance, reporting, and research efforts.
As of 2025, the most recent comprehensive data indicate that the biennial pattern of AFM outbreaks was disrupted during the COVID-19 pandemic years (2020–2022), likely due to widespread public health interventions such as masking, social distancing, and school closures, which reduced the circulation of respiratory viruses implicated in AFM pathogenesis. However, with the relaxation of these measures and the resumption of typical social interactions, experts anticipate a resurgence in AFM cases, potentially returning to or exceeding pre-pandemic levels. The CDC’s surveillance data suggest that the number of confirmed AFM cases in 2023 and early 2024 has begun to rise, aligning with historical trends and supporting forecasts of increased incidence in the coming years.
Globally, the World Health Organization (WHO) has recognized AFM as a condition of concern, particularly in regions with robust enterovirus circulation. While the United States has the most comprehensive AFM surveillance system, other countries are increasingly reporting cases, suggesting that AFM may be underrecognized in areas with less developed healthcare infrastructure. The WHO continues to encourage member states to strengthen surveillance and reporting mechanisms to better understand the global epidemiology of AFM.
Looking ahead to 2025 and beyond, modeling studies and expert consensus anticipate a 15–25% increase in public attention to AFM, driven by heightened awareness, improved diagnostic capabilities, and the potential for larger outbreaks as population immunity to enteroviruses fluctuates. The CDC and WHO are expected to expand their outreach and educational campaigns, while research into the etiology, prevention, and treatment of AFM is likely to accelerate. The outlook for AFM incidence through 2030 remains uncertain, but the consensus among public health authorities is that vigilance and preparedness will be essential to mitigate the impact of future outbreaks.
Future Outlook: Research Priorities and Global Preparedness
Acute Flaccid Myelitis (AFM) has emerged as a significant public health concern due to its unpredictable outbreak patterns and potential for severe neurological impairment, particularly in children. Since its initial recognition in 2014, AFM has demonstrated a biennial pattern of increased incidence, with notable spikes in the United States in 2014, 2016, and 2018. However, this pattern was disrupted in 2020, likely due to the widespread implementation of non-pharmaceutical interventions (NPIs) such as social distancing and mask-wearing during the COVID-19 pandemic, which also reduced the circulation of enteroviruses commonly associated with AFM, such as enterovirus D68 (EV-D68).
As of 2025, surveillance data indicate that AFM cases remain below pre-pandemic levels, but experts caution that the risk of future outbreaks persists as NPIs are relaxed and enterovirus transmission resumes. The Centers for Disease Control and Prevention (CDC), the primary public health authority in the United States, continues to monitor AFM trends through its national surveillance system and collaborates with state health departments to rapidly identify and investigate suspected cases. The CDC’s most recent updates suggest that while 2023 and 2024 saw only sporadic cases, the potential for a resurgence in 2025 and subsequent years remains, particularly if EV-D68 or other neurotropic enteroviruses circulate widely.
Globally, the World Health Organization (WHO) has recognized AFM as a condition of interest, especially in regions with limited surveillance infrastructure. International data remain sparse, but there is growing concern that underreporting may mask the true burden of AFM outside North America and Europe. The WHO is working to strengthen global surveillance and laboratory capacity to improve detection and response to AFM outbreaks.
Looking ahead, research priorities include elucidating the precise mechanisms by which enteroviruses cause AFM, developing rapid diagnostic tools, and advancing vaccine candidates targeting implicated viruses such as EV-D68. The CDC and WHO have both emphasized the importance of international collaboration to share data, harmonize case definitions, and coordinate outbreak response strategies. As travel and social interactions return to pre-pandemic norms, public health authorities anticipate that AFM incidence may rise, underscoring the need for continued vigilance, investment in research, and preparedness planning to mitigate the impact of future outbreaks.
Sources & References
- Centers for Disease Control and Prevention
- World Health Organization
- National Institutes of Health (NIH)